Error message
Warning: Undefined array key 0 in dom_theme_suggestions_we_megamenu_submenu_alter() (line 41 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_submenu_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 82) __TwigTemplate_1e1012ecb907286344b2e8f4bed56b75->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_41a70b48747e986c61f6990c6b2c425f->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_cd888e044ffdd7a1ff22e98aa67fb5b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Trying to access array offset on null in dom_theme_suggestions_we_megamenu_submenu_alter() (line 41 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_submenu_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 82) __TwigTemplate_1e1012ecb907286344b2e8f4bed56b75->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_41a70b48747e986c61f6990c6b2c425f->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_cd888e044ffdd7a1ff22e98aa67fb5b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Undefined array key 0 in dom_theme_suggestions_we_megamenu_col_alter() (line 29 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_col_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 82) __TwigTemplate_1e1012ecb907286344b2e8f4bed56b75->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_41a70b48747e986c61f6990c6b2c425f->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_cd888e044ffdd7a1ff22e98aa67fb5b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Trying to access array offset on null in dom_theme_suggestions_we_megamenu_col_alter() (line 29 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_col_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 82) __TwigTemplate_1e1012ecb907286344b2e8f4bed56b75->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_41a70b48747e986c61f6990c6b2c425f->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_cd888e044ffdd7a1ff22e98aa67fb5b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Undefined array key 0 in dom_theme_suggestions_we_megamenu_submenu_alter() (line 41 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_submenu_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 82) __TwigTemplate_1e1012ecb907286344b2e8f4bed56b75->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_41a70b48747e986c61f6990c6b2c425f->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_cd888e044ffdd7a1ff22e98aa67fb5b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Trying to access array offset on null in dom_theme_suggestions_we_megamenu_submenu_alter() (line 41 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_submenu_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 82) __TwigTemplate_1e1012ecb907286344b2e8f4bed56b75->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_41a70b48747e986c61f6990c6b2c425f->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_cd888e044ffdd7a1ff22e98aa67fb5b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Undefined array key 0 in dom_theme_suggestions_we_megamenu_col_alter() (line 29 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_col_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 82) __TwigTemplate_1e1012ecb907286344b2e8f4bed56b75->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_41a70b48747e986c61f6990c6b2c425f->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_cd888e044ffdd7a1ff22e98aa67fb5b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Trying to access array offset on null in dom_theme_suggestions_we_megamenu_col_alter() (line 29 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_col_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 82) __TwigTemplate_1e1012ecb907286344b2e8f4bed56b75->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_41a70b48747e986c61f6990c6b2c425f->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_cd888e044ffdd7a1ff22e98aa67fb5b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Undefined array key 0 in dom_theme_suggestions_we_megamenu_submenu_alter() (line 41 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_submenu_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Trying to access array offset on null in dom_theme_suggestions_we_megamenu_submenu_alter() (line 41 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_submenu_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Undefined array key 0 in dom_theme_suggestions_we_megamenu_col_alter() (line 29 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_col_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Trying to access array offset on null in dom_theme_suggestions_we_megamenu_col_alter() (line 29 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_col_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Undefined array key 0 in dom_theme_suggestions_we_megamenu_col_alter() (line 29 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_col_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Trying to access array offset on null in dom_theme_suggestions_we_megamenu_col_alter() (line 29 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_col_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Undefined array key 0 in dom_theme_suggestions_we_megamenu_submenu_alter() (line 41 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_submenu_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 82) __TwigTemplate_1e1012ecb907286344b2e8f4bed56b75->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_41a70b48747e986c61f6990c6b2c425f->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_cd888e044ffdd7a1ff22e98aa67fb5b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Trying to access array offset on null in dom_theme_suggestions_we_megamenu_submenu_alter() (line 41 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_submenu_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 82) __TwigTemplate_1e1012ecb907286344b2e8f4bed56b75->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_41a70b48747e986c61f6990c6b2c425f->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_cd888e044ffdd7a1ff22e98aa67fb5b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Undefined array key 0 in dom_theme_suggestions_we_megamenu_col_alter() (line 29 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_col_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 82) __TwigTemplate_1e1012ecb907286344b2e8f4bed56b75->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_41a70b48747e986c61f6990c6b2c425f->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_cd888e044ffdd7a1ff22e98aa67fb5b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Trying to access array offset on null in dom_theme_suggestions_we_megamenu_col_alter() (line 29 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_col_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 82) __TwigTemplate_1e1012ecb907286344b2e8f4bed56b75->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_41a70b48747e986c61f6990c6b2c425f->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_cd888e044ffdd7a1ff22e98aa67fb5b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Undefined array key 0 in dom_theme_suggestions_we_megamenu_col_alter() (line 29 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_col_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 82) __TwigTemplate_1e1012ecb907286344b2e8f4bed56b75->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_41a70b48747e986c61f6990c6b2c425f->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_cd888e044ffdd7a1ff22e98aa67fb5b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)Warning: Trying to access array offset on null in dom_theme_suggestions_we_megamenu_col_alter() (line 29 of sites/medicine.ucsf.edu/themes/custom/dom/dom.theme).
dom_theme_suggestions_we_megamenu_col_alter() (Line: 458) Drupal\Core\Theme\ThemeManager->alterForTheme() (Line: 467) Drupal\Core\Theme\ThemeManager->alter() (Line: 394) Drupal\Core\Theme\ThemeManager->buildThemeHookSuggestions() (Line: 220) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 82) __TwigTemplate_1e1012ecb907286344b2e8f4bed56b75->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_41a70b48747e986c61f6990c6b2c425f->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 44) __TwigTemplate_cd888e044ffdd7a1ff22e98aa67fb5b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_e725d3f3676970c39d512256a3600b39->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_96f878a02edb7be76cb7d94cc693b46e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_0223e07f8797c2da5b7b60503c65c5a0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_812abb86c4ae93f4ad0abb54f4508c6e->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 50) __TwigTemplate_61438b60cb62312c070272e7a78f8b54->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 80) __TwigTemplate_9e79c449e0c0612f5a338b1c77955fa1->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 47) __TwigTemplate_2efd3f9116558ffd2f95eee94cb78cee->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 49) __TwigTemplate_39f113f734e333e145c8cb7e21216aef->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 100) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->block_content() (Line: 432) Twig\Template->yieldBlock() (Line: 83) __TwigTemplate_ae8d64d0832b14a025c6258cdc6a54b8->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 504) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 72) __TwigTemplate_5693c790dabc2db57a2f5badf9bea9e0->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 484) Drupal\Core\Template\TwigExtension->escapeFilter() (Line: 99) __TwigTemplate_3d3fee7c344d8290941ce227bf7f1f46->doDisplay() (Line: 388) Twig\Template->yield() (Line: 344) Twig\Template->display() (Line: 359) Twig\Template->render() (Line: 51) Twig\TemplateWrapper->render() (Line: 33) twig_render_template() (Line: 348) Drupal\Core\Theme\ThemeManager->render() (Line: 491) Drupal\Core\Render\Renderer->doRender() (Line: 248) Drupal\Core\Render\Renderer->render() (Line: 158) Drupal\Core\Render\MainContent\HtmlRenderer->Drupal\Core\Render\MainContent\{closure}() (Line: 638) Drupal\Core\Render\Renderer->executeInRenderContext() (Line: 153) Drupal\Core\Render\MainContent\HtmlRenderer->renderResponse() (Line: 90) Drupal\Core\EventSubscriber\MainContentViewSubscriber->onViewRenderArray() call_user_func() (Line: 111) Drupal\Component\EventDispatcher\ContainerAwareEventDispatcher->dispatch() (Line: 186) Symfony\Component\HttpKernel\HttpKernel->handleRaw() (Line: 76) Symfony\Component\HttpKernel\HttpKernel->handle() (Line: 53) Drupal\Core\StackMiddleware\Session->handle() (Line: 48) Drupal\Core\StackMiddleware\KernelPreHandle->handle() (Line: 28) Drupal\Core\StackMiddleware\ContentLength->handle() (Line: 48) Drupal\Core\StackMiddleware\ReverseProxyMiddleware->handle() (Line: 51) Drupal\Core\StackMiddleware\NegotiationMiddleware->handle() (Line: 36) Drupal\Core\StackMiddleware\AjaxPageState->handle() (Line: 51) Drupal\Core\StackMiddleware\StackedHttpKernel->handle() (Line: 741) Drupal\Core\DrupalKernel->handle() (Line: 19)
Health Policy & Advocacy

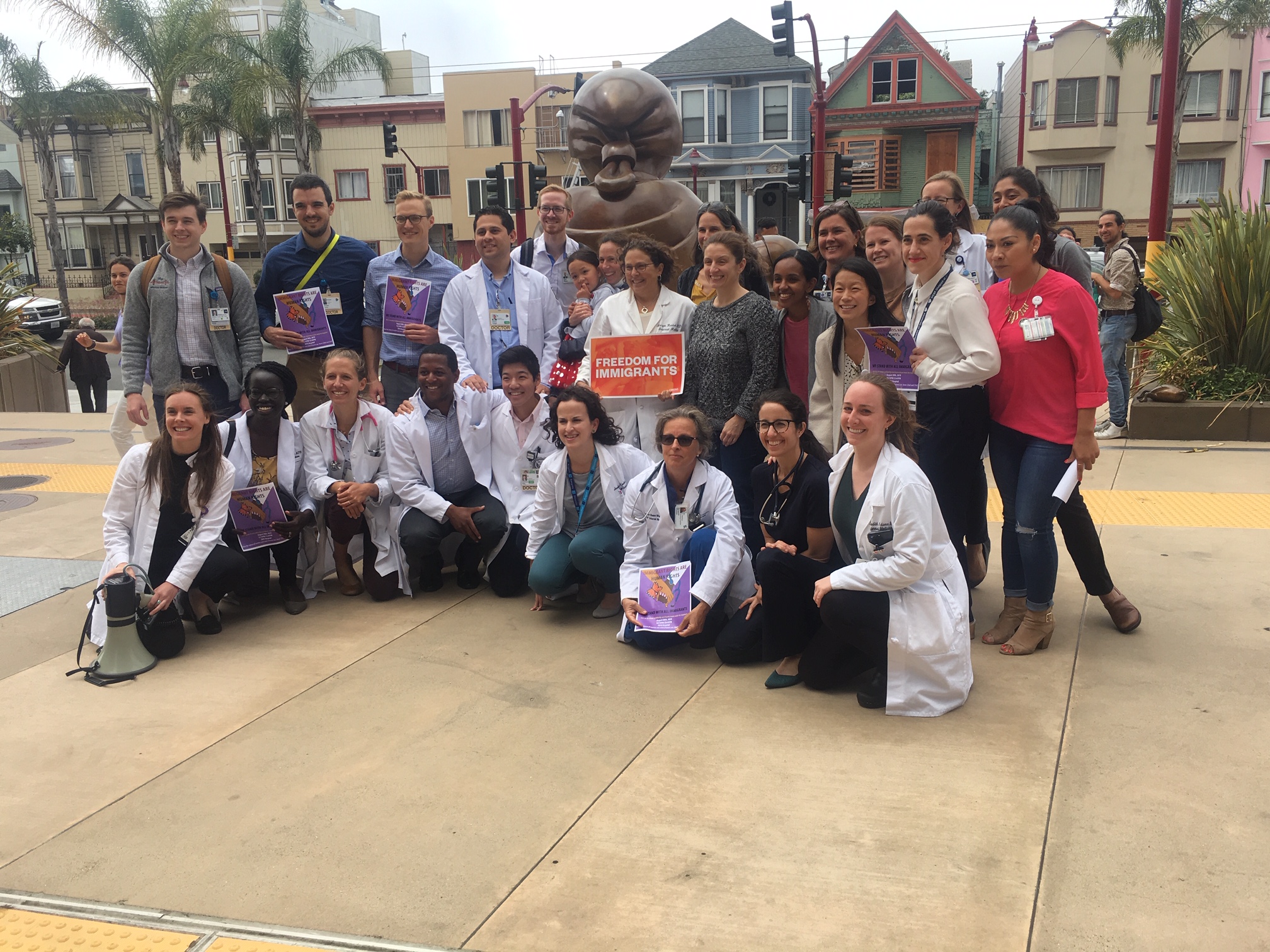

Health policy work conducted in the Division of General Internal Medicine is unified by a firm commitment to improve conditions and policies to enhance the health and well-being of vulnerable populations. Listed below are descriptions of some of our faculty members' current policy work.
Soraya Azari, MD
Dr. Azari’s health policy interest relates to the use of opioid medications for treatment of chronic, non-cancer pain. She is part of a working group comprised of San Francisco safety net providers who aim to devise best practices for use of opioids in primary care. Her group has drafted quality standards for participant clinics, and is collaborating with local emergency departments to discuss appropriate use of opioids.
Kirsten Bibbins-Domingo, MD
Dr. Bibbins-Domingo current work focuses on understanding the interaction between social, behavioral, and biological factors that place vulnerable groups at risk for cardiovascular disease early in life and population-wide policy level interventions that may prevent disease in these groups. She has provided recommendations to local, state, federal, and international organizations interested in the impact on food and nutrition policies on cardiovascular disease prevention and health disparities, including the California Department of Public Health, the Centers for Disease Control and Prevention (CDC), and the Pan American Health Organization (PAHO). She has served on several committees of the Institute of Medicine (IOM), advising federal agencies on policies related to adverse effects of vaccines, presumptive disability in veterans, valuing community-based prevention, and evaluating the impact of population-wide sodium reduction. She is a member of the US Preventive Services Task Force that develops national guidelines for clinical prevention.
Maria Chao, MD
Dr. Chao’s policy and advocacy efforts focus on improving access to evidence-based complementary and integrative medicine for underserved populations. Her current work includes broadening non-pharmacologic options for pain management in primary care and evaluating the implementation of acupuncture in safety net settings to improve quality of life among patients with chronic conditions. She has published on racial/ethnic differences in reasons for using complementary health approaches, factors that affect disclosure of complementary medicine use to healthcare providers, and socioeconomic access to integrative health through group-based models. Dr. Chao is a member of the steering committee for the Integrative Pain Management Program of the San Francisco Health Network. She co-chairs a Working group on Traditional and Complementary Medicine Research in Asian American Communities and serves on the Board of Directors Integrative Medicine for the Underserved, a national multi-disciplinary organization committed to affordable, accessible integrative health care for all.
Alicia Fernandez, MD
Dr. Fernandez’s policy work has primarily focused on issues affecting US minority and immigrant populations related to chronic disease care. She is particularly interested in language barriers in health care and the associated policy implications regarding physician language ability and professional interpreter use. Her work in this area has included research on: the impact of language barriers on the management of Type 2 diabetes among Latinos; resident physicians’ use of professional interpreters; the accuracy of tools used to assess physicians’ self-reported Spanish language ability; and the need for national training and certification standards for professional health care interpreters. She has served as an advisor to numerous national foundations, the AMA, ABIM, and other stakeholders focused on health disparities and to state and national advisory committees focused on language barriers and cultural competence. Dr. Fernandez served on the Society of General Internal Medicine Council (2006-09). In addition to her research-related policy work, Dr. Fernandez serves on the board of trustees of American Civil Liberties Union-Northern California.
Liz Goldman, MD
Dr. Goldman’s research and policy work focuses on improving the quality of health care for underserved communities and the safety-net in particular. She promotes high quality, cost-conscious, and appropriate care in the safety-net, and evaluates innovations and health delivery approaches to improve care transitions and provider communication across settings and specialties. As part of her work to improve the science of quality measurement, she has served on an expert work group for Agency for Healthcare Research and Quality Present on Admission (POA) Project.
Claire Horton, MD
Dr. Horton's policy and advocacy work centers on primary care re-design in safety net settings, the elimination of racial and ethnic disparities through primary care quality improvement (QI) efforts, and coaching physician leaders to create system-level change. She launched and co-directs (with Dr. Urmimala Sarkar) the "Triple AIM" curriculum for primary care internal medicine residents at SFGH. The curriculum introduces residents to core QI concepts and skills and includes an experiential component in which residents complete clinic-based QI projects. She is part of UCSF/Center for Health Professions' ACTION grant network, which focuses on integration of health disparities data into QI initiatives. She serves on the advisory board for Healthy San Francisco / San Francisco Health Plan's Quality Improvement initiatives, which have been instrumental in helping to create Pay-for-Performance initiatives in the San Francisco safety net. In the past she has also served on California's Medicaid Managed Care advisory board. She is a coach for the UCSF Center for Health Professions' Institute for Physician Leadership, which aims to equip California's physician leaders with leadership skills to lead their organizations and create meaningful change in statewide healthcare systems (http://www.futurehealth.ucsf.edu/Public/Leadership-Programs/Home.aspx?pid=65)
Leigh Kimberg, MD
Dr. Leigh Kimberg’s policy and advocacy work focuses on violence prevention, increasing enrollment of medical students from historically excluded communities, and advancing anti-racist, anti-oppression health professions education. She has worked on policy and advocacy initiatives to prevent and mitigate the adverse effects of violence and trauma and promote models of healing-centered, trauma-informed healthcare. Dr. Kimberg has served on national advisory boards convened by Futures without Violence (previously the Family Violence Prevention Fund) to develop national guidelines on addressing intimate partner violence in healthcare practice; she has also advocated for these guidelines to be adopted and implemented locally. She garnered federal funding to study the implementation of the Affordable Care Act’s mandate to provide all girls and women with IPV counseling and services. Dr. Kimberg serves as the San Francisco Department of Public Health (SFDPH) representative to the Board of Supervisors mandated San Francisco Family Violence Council (SF FVC) to advance violence prevention and intervention policies in collaboration with other governmental and community-based organization partners. Recently, Dr. Kimberg has been engaging in abolitionist advocacy to eliminate policing in healthcare, including in SFDPH. As the Program Director for Program in Medical Education for the Urban Underserved (PRIME-US) at UCSF and the UCB-UCSF Joint Medical Program, she participates in policy and advocacy efforts to recruit and equip students from historically excluded communities to become physician health equity leaders. She is also privileged and honored to have the opportunity to actively support the policy and advocacy efforts of the PRIME-US students, who are national leaders in many areas including anti-racist medical education and healthcare, access to care, immigrant’s rights, DACA, and more.
Margot Kushel, MD
Dr. Kushel’s policy work focuses on addressing housing as a key social determinant of health. Her work aims to create the evidence base for policy responses to prevent and end homelessness and mitigate the effects of housing instability on health. Dr. Kushel works with diverse stakeholders at the local, regional, and national level to inform and implement programmatic and policy changes based on her research, which focuses on the causes and consequences of homelessness in older adults and the effects of various housing interventions on health care utilization and health outcomes. She has provided testimony at California state legislative committees, presented her findings at local, regional, and national conferences, and is a frequent speaker to medical and lay audiences on highly vulnerable populations both in person and through traditional and new media. She is a leadership board member of Everyone Home, which coordinates homeless policy in Alameda County. She serves as an evaluator of multiple initiatives seeking to address homelessness, including Santa Clara’s Pay for Success funded supportive housing initiative, Tipping Point’s Chronic Homelessness Initiative and Whole Person Care in San Francisco.
Courtney Lyles, PhD
Dr. Lyles’s policy work currently focuses on health information technology implementation and digital inclusion, specifically patient engagement and digital/health literacy among vulnerable populations. Dr. Lyles advocates for the design and dissemination of better health information technology tools for vulnerable patients, through better skills training and support, increased usability standards, and metrics that demonstrate true patient engagement. Here are a few recent highlights:
Focusing on Digital Health Equity (JAMA Viewpoint)
Tackling digital inequality in the tech capital of the world (SF Examiner)
Nynikka Palmer, PhD
Dr. Palmer’s policy and advocacy efforts are centered around achieving health equity for high-quality care for African American men facing prostate cancer. Her work sits at the intersection of multiple fields and methods, including cancer disparities, health services research, health care communication, and community engagement. She launched an African American prostate cancer support group, as none existed in the Bay Area, with the mission to provide a safe and supportive place where men can come together for dialogue and education. With a roster of over 90 African American men, this group has been thriving since 2014. As co-leader of the SF CAN Prostate Cancer Task Force, the group is leading efforts for Smarter Screening and Smarter Treatment for prostate cancer, to eliminate sub-optimal screening practices and treatment in African American men through community and health care system partnerships.
Neda Ratanawongsa, MD
Dr. Ratanawongsa's advocacy work has focused on system redesign to support safety net clinicians in developing meaningful therapeutic alliances with their patients. Specifically, she is interested in assuring that quality measures, incentives, and health system policies promote relationship-centered communication, support clinician well-being, and improve the recruitment and retention of diverse clinicians in the safety net workforce. Dr. Ratanawongsa's current focus is on tailoring electronic health record system implementation metrics to meet the needs of clinicians caring for linguistically and culturally diverse populations.
Urmimala Sarkar, MD
Dr. Sarkar’s policy and advocacy work focus on the areas of patient safety, specifically for vulnerable populations with chronic conditions, and health information technology. She serves as an advisor to the National Patient Safety Foundation on outpatient issues and recently served on a Technical Expert Panel on ambulatory safety for the U.S. Department of Health and Human Services. In addition, Dr. Sarkar is passionate about harnessing the health information technology revolution to reduce racial/ethnic, economic, and literacy-related disparities in health care by innovating to address the unmet need for appropriate patient-facing technologies for vulnerable populations.
Dean Schillinger, MD
Dr. Schillinger has a long history of successfully advocating for healthcare and public health policies to enhance health communication for health equity in a variety of domains, including patient safety, health literacy, and digital communication. Dr. Schillinger is also a leading scientific and public health expert on the root causes of the global diabetes epidemic and has been instrumental in engaging the scientific community in the critical policy discourse related to the dangers of unmitigated added sugar consumption. Because of his diabetes public health expertise, he served as the scientific expert for the City and County of San Francisco in the successful defense of a lawsuit filed in Federal Court by the American Beverage Association for an injunction against a city ordinance to mandate health warning labels on billboards advertising sugary drinks. As a result of the City’s successful defense, the first sugary drink warning label law in the world will go into effect in 2017 (1) requiring health warnings on advertisements for sodas and other sugary drinks (2) banning such advertising on city property and (3) prohibiting the city from spending money on sugary drinks. Dr. Schillinger has recently authored a number of widely-read original investigations as well as influential public health policy pieces in the Annals of Internal Medicine and JAMA that describe how the sugary beverage industry has been manipulating disparate elements of the scientific process to undermine scientific claims of their products’ health consequences and to create controversy regarding the scientific basis for placing dietary limits on added sugars. To directly engage the affected communities in the emerging crisis of Type 2 diabetes in America’s children, Dr. Schillinger co-created a minority youth-led public health literacy campaign to prevent diabetes that employs social media and spoken word, The Bigger Picture (http://www.thebiggerpicture.org/), which was highlighted at a 2013 IOM Health Literacy Policy Roundtable event, was awarded the Spirit of 1848 Award from the American Public Health Association and recently received the WHO NCD Policy Innovations Award. An innovative marriage of Public Health and the Arts, The Bigger Picture has been evaluated by his team, and results demonstrate its positive impacts on minority youth and youth stakeholders. The Bigger Picture campaign has had >1.5 million views to date, has been adopted by 3 California counties for their initiatives to reduce sugar-sweetened beverage consumption, and was influential in the passage of sugary drink taxation policies in 4 Bay Area municipalities through its engagement of minority voters. In 2016, Dr. Schillinger received the prestigious James Irvine Leadership Award of California for his groundbreaking work in advancing the public health literacy of Californians with respect to the diabetes epidemic. Dr. Schillinger has also served as a consultant to Navajo Nation, the Ministry of Health in Israel regarding their diabetes prevention efforts, and to the Ministry of Health in Singapore after it declared a “War on Diabetes”. His efforts led to Singapore becoming the first nation in the world to ban advertising of sugary drinks. Finally, Dr. Schillinger served as co-chair of the Congressionally-chartered National Clinical Care Commission whose purpose was to prepare and submit a report on how US federal agencies can be better leveraged to prevent and control diabetes. He was in charge of the sub-committee making recommendations on all non-health agencies (e.g. HUD, USDA, Dept of Education, FTC, etc.) on behalf of an all-government approach to diabetes prevention and control.
Hilary Seligman, MD
Dr. Seligman’s policy and advocacy expertise focus on federal nutrition programs (predominantly the Supplemental Nutrition Assistance Program), community food programs (food vouchers, food banks, and food pantries), food affordability and access, and income-related drivers of food choice. She serves as Senior Medical Advisor for Feeding America, the nation’s largest domestic anti-hunger organization. She directs the CDC’s Nutrition and Obesity Policy Research and Evaluation Network (www.nopren.org). She also founded San Francisco’s fruit and vegetable voucher program, EatSF (eatsfvoucher.org), which has since expanded to other cities as Vouchers for Veggies.
Maya Vijayaraghavan, MD
Dr. Vijayaraghavan’s policy work is focused on tobacco control policy, with an emphasis on vulnerable populations. She analyzes national cross-sectional and longitudinal data to examine the differential impact of tobacco control policies on low-income populations in the US. Dr. Vijayaraghavan is interested in the implementation of smoke-free policies in subsidized housing, including permanent supportive housing for persons who were formerly homeless and for other forms of subsidized housing including Housing Choice Vouchers or subsidized housing in the private rental market. She is currently the PI of a grant funded by the National Cancer Institute on conducting a cluster randomized controlled trial of a smoke-free home intervention in permanent supportive housing for formerly homeless in the San Francisco Bay Area. Dr. Vijayaraghavan’s broader tobacco control policy work also encompasses system-level approaches to increase access to cessation services for low-income populations in the US. She is the PI of a grant funded by the Tobacco Related Disease Research Program to conduct a pilot randomized controlled trial of a contingency management intervention for patients experiencing homelessness who are engaged in clinical care at the Tom Waddell Urban Health Clinic in San Francisco, CA. This intervention is integrated within the clinic’s Epic electronic health record. She is also a co-investigator on a grant funded by the Tobacco Related Disease Program on developing system level approaches using the electronic health record to increase delivery of cessation services to patients in safety net health systems. Using these approaches, her team has developed ways to estimate quit attempts at population level among primary care patient populations as well as integrating health systems with population-level interventions such as the state tobacco quitline. Her most recent project is focused on the integration of smoking.